Posted 1315 days ago
SHALIN SHAH, DMD, MS
Orthodontic treatment objectives are well established for sagittal and vertical dimensions in terms of how teeth and jaws should be related, fitting and working together. The diagnostic and treatment strategies that focus on these dimensions are the issue of many symposia, conferences and orthodontic research work. However, the transverse dimension is missing the analysis and discussions of generally accepted and performance patients. In addition, the well -defined criteria to determine whether it is necessary to be based on the correction on the objective average, instead of subjective, are often not used.
As there are treatment objectives for the final positions of the tooth based on sagittal and vertical skeletal dimensions, there must be a set of objectives defined for transversal. For the posterior teeth, the thesis would be to have in an upright position and centered on the alveolus in addition to being well interacted with the proper coordination of the arch, as shown in Figure 1.
Figure 1: Position of the posterior tooth
When there is a skeletal transverse discrepancy, sometimes, this is recognized by a posterior dental bite. However, there are many times no posterior dental bite, but maxillary posterior teeth are built, and mandibular posterior teeth are inclined lingual to compensate for skeletal disharmony. This compensated dental arrangement opens the patient to a great probability of non -work interference of lunch palatal cups, centered prematurities and functional changes, in addition to placing forces outside the axis in the dentition. The “decompensation” that faces and focuses on the alveolus, then revives the “skeletal transverse bite” “underlying and the amount of skeletal correction required, as shown in Figure 2.
Figure 2: Ideal, compensated, decompensated relationship
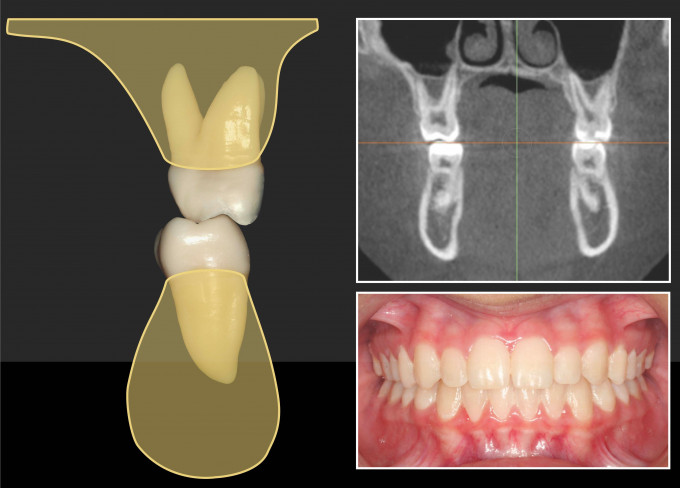
While it is possible to achieve a good rectifier and intercuspation of the posterior teeth in the presence of a lack of skeletal harmony, the risk of doing so is a potential commitment to the periodoncio. In an attempt to stand and interest the teeth well in the presence of a discrepancy, the amount of soft and bone tissue on the roots becomes thinner (Figure 3) The teeth will no longer focus on the alveolus. In minor discrepancies, the effects of this dental positioning may not represent a group. However, in serious transverse discrepancies, an attempt to normalize the inclination of posterior dentition and intercuspation in the light of the lack of non -pointed skeletal harmony, the fenestration of the root and the loss of clinicular obese attacks, as present in the figure.
Figure 3: thinner tissue and bone in maxilla Tooth
Figure 4 Root fenestration and loss of attachment
Moderate skeletal discrepancies are the most common lost situation using only clinical observation and not an objective analysis. However, a practitioner can appreciate where a underlying skeletal bite is present, in the absence of a dental, observing the inclinations of the mandibular teeth (Figure 5).
Figure 5 The inclination of mandibular teeth
In these scenarios, the consequences of the standardization of the position of the tooth, without skeletal correction, and its effect on long -term periodontal viability may not be performed clinically. In the debit, it may seem that the posterior teeth were corrected with only the use of supports, crossed elastic or expanded arches. However, because no loss of heel was observed during treatment, the practitioner can erroneously assume that the patient was not damaged or that the periodoncio is viable and resistant in the long term.
Approximately time and in a susceptible patient, as indicated above, the gingival union can be less resistant to normal tensions that are placed due to most of the tissue in the face of the amount present in a non -commitment patient. There is now a high risk of periodontal tissue loss induced by mechanics, as special for those patients who may have a thinner tissue biotype at the beginning. Therefore, negative sequelae of loss of attachment and recession may not appear until years or decades later, depending on adaptability, periodontal biotype of the patient and genetic composition2.